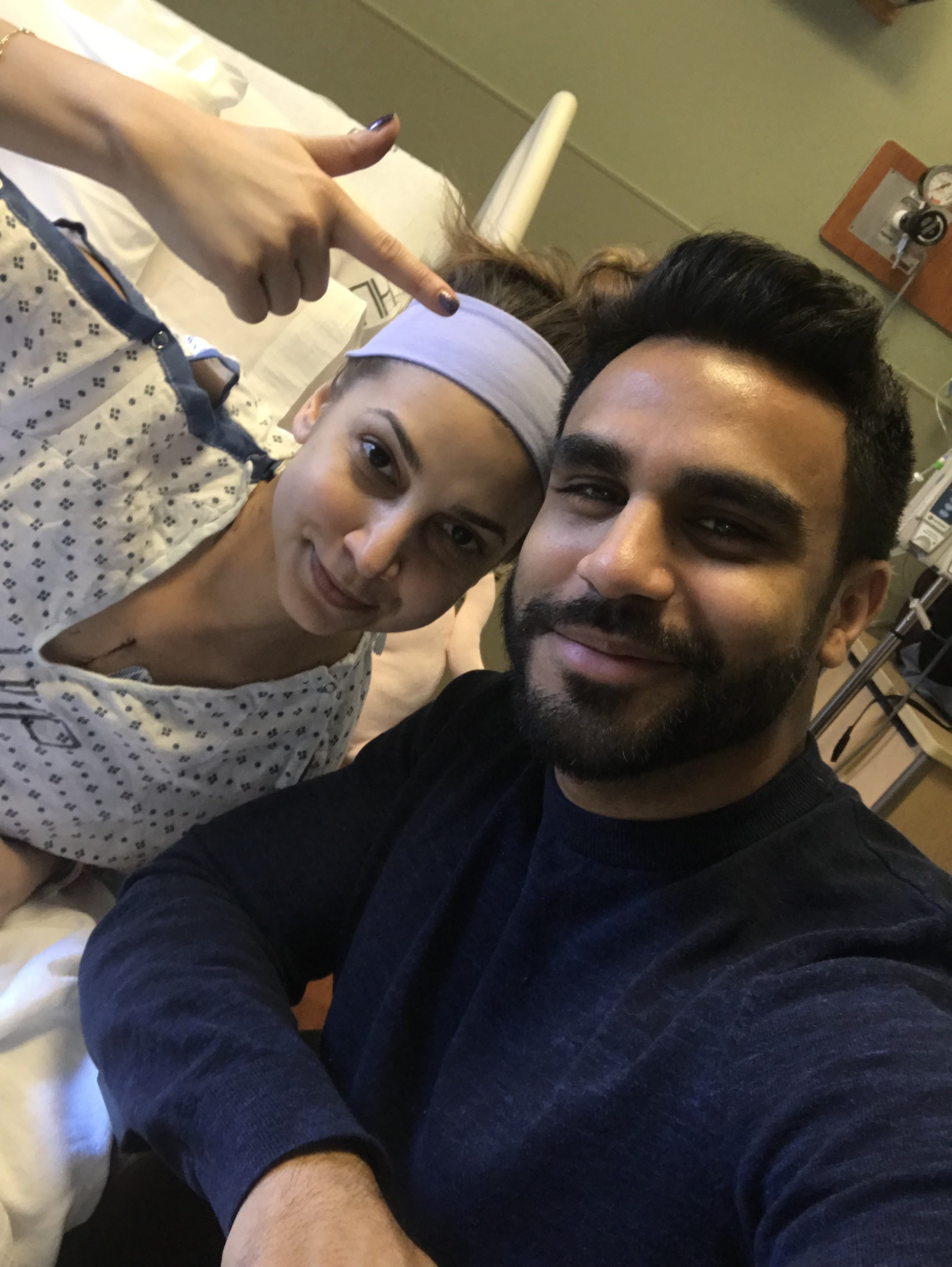
Doctor-Patient Alin
What is it like being a transplant patient and an ER resident at the same time?
Well, let me tell you:
I guess it’s the little things that matter, like working in that one pod with the bathroom closest to the doctor’s station is a lot easier than working in the other pods. Sometimes, my medications make me really nauseous and I just feel like I have to throw up. Mostly though, drinking all that water every day because in the back of my mind, I am constantly thinking about my creatinine level (i.e. Tacrolimus probably slowly killing my kidneys, one pill at a time, as I check my BUN:Cr ratio over and over again)... that’s a lot of trips to the bathroom.
Speaking of, it’s hard to remember to drink a lot of water during those busy ER shifts. Start a note. Sip of water. Look at an EKG. Sip of water. See a patient, return to desk, sip of water. Finish water, throw it out, forget to get more water. Damnit. I actually had to download an app that reminds me to hydrate more every day. It’s been going well. ;)
If my Transplant Team calls, I have to take the call. They are on Emergency Bypass on my cell phone. And sometimes, there are mix-ups. Ahem:
“Yeah okay so labs are good, we’ll do an echo, got it thanks bye,” I say quickly, on the phone.
“Was that about our patient in 3, Alin?” asks my attending.
“No, that was about me.”
And so on and so forth.
Sometimes, I’ll be in the middle of seeing a patient and my medication alarm will go off. Tacrolimus time. A little battle in my head ensues: rejection (my own preventable demise) vs. patient care (I do care, I promise). Sometimes, I say I will be right back. Other times, I will wait a few more moments until my patient finishes up their story. Quick physical exam. Lungs CTAB, gotta go get my Tac, will be back to finish exam. I guess it depends on the situation. I’ve mostly discovered that the best way to go about this is to just try to NOT be in a patient’s room around 9am and 9pm. Very strategically.
This is difficult in the emergency department, as people can go into respiratory distress or cardiac arrest at any time of day, at any moment in their lives. Trust me. I know.
Another thing: I know that I probably look funny. I have a mask on at all times. Some patients ask me if I’m sick and I say, “No, I just have a heart transplant, no big deal.” All have been shocked by this reply. Some have thanked me for being open about my transplant (or apologetic for asking).
Some don’t really hear my muffled voice under the mask unless they have their hearing aids in (naturally, they might have forgotten them at home). This becomes a major problem, so our nurses have to help me out with getting a thorough history.
One patient said that his own chest pain resolved after I told him why I was wearing the mask. And thennnnnnn he said something like, “Sure hope I don’t ever need one of those. Damn.” We both nervously chuckled.
I have to bring my own pens to work, and awkwardly disinfect everything my attendings and colleagues touch. I get really antsy when we have to keep switching work stations. “Can we just have a rule where the immunocompromised resident just gets to sit at the work station she disinfected for five minutes straight?” I once asked, laughingly. (This is essentially impossible at times in busy, academic ERs).
I carry Purell with me in my pocket. On my desk. In my backpack. Purell here, there, everywhere. Before, after, during seeing patients, talking to attendings, typing notes, walking to the suture cart, getting ready to leave, you name it. I use hand sanitizer so often that my hands officially look like dry, reptilian claws. I use hand sanitizer so often that I think Purell should just sponsor me. Hey Purell. I’m here.
Nurses and residents and attendings ask me things like, “How did it feel when...” and “What was the worst part about...” and no, it never gets old. I am raw and honest and I hope that they appreciate that. Sometimes, a clinical pearl or two is thrown around, all thanks to my dry humor— “Remember, no Atropine for me if I ever brady down, guys!”
And sometimes, I just have to sit down for a second. To think. I do this thing where I just stare down at my desk like a zombie (truly). Sometimes I close my eyes. Just a 30 second break. I only recently started working clinically. There is an emotional component that goes with all of this. If you only knew what it felt like the first time I heard the sound of someone getting suctioned after we emergently intubated them...
Of course, some patients do say things like, “Ah you are so young, wait until you are old and have been through what I’ve been through” or “You don’t know what it’s like to be so sick.”
I mutter, “I know, I know.” Sometimes, I wish that they knew. I can’t tell every single patient my story.
When a coding patient comes in through the doors, it’s more than just a code to me.
What I see in front of me is just another person, like you and me, who’s most vital organ has failed on them. This vital organ— the heart— capable of beautifully beating just so many times in a person’s life (I once heard about 3 billion times per average lifespan) has stopped, for whatever reason. It is now up to us to try to pump the body with blood, perfuse the organs with oxygen—with rhythmic compressions of the chest, one one thousand, two one thousand, three one thousand...
Until the heart decides: can they fix this, or am I broken for good?
Until the heart decides if it is done doing its job.
The heart *is* the most vital organ of the body. If it decides that it does not want to continue beating, after all of our efforts (and trust me on those efforts), our patient is officially dead. And just like that, in the blink of an eye, in less than a nanosecond, they are gone. Everything that they had lived for, their unforgettable presence in this world, their lovely soul ... is gone.
The heart can abruptly stop working on anybody. I have seen it all. Young, old, previously healthy, unhealthy, those with traumatic injuries, those without. Because although there are risk factors for most heart diseases, sometimes there just aren’t.
These particular moments have become extremely eye-opening for me.
And then, of course, I can’t help but think: holy shit, that could have been me.
And it’s not like I didn’t know this before. But seeing this again after my transplant surgery reminds me of how lucky I am to have been given a second one of these vital little things. Vital little powerful things.
I hope that it has enough beats left to beat away for the rest of my crazy life. I am living on borrowed time, right? Every single borrowed heartbeat is so precious to me. So phenomenal, so amazing. I still can’t believe it. It has been ten months, and I still can’t believe it.
So ... what *is* it like being a transplant patient and an ER resident at the same time?
It’s awkward and hilarious and endearing. It’s frustrating. It has made me connect with patients on a whole new level. It has taught my colleagues a thing or two about transplants.
But overall, it has made me so much more grateful of everything that has happened to me this year. Making those terrible moments— those tougher days, the pain, the lab draws, the headaches, the restrictions— seen so minute compared to what could have been....
Nice to be writing again. ;)
I’ll be trying to do blogposts (or at least updates) every other weekend. Always feel free to email me at contact.changeofheart@gmail.com if you need anything. ❤️
And with that:
“I have no choice of living or dying, you see, sir-- but I do have a choice of how I do it.”
John Steinbeck, The Moon Is Down